Leveraging Strengths to Improve Asthma Care
Associate Professor Edgar Lobaton is working with UNC researchers on an NSF-funded project to improve wearable health-monitoring devices so that they may one day be able to help asthma patients manage their symptoms better.
October 10, 2019 ![]() Staff
Staff
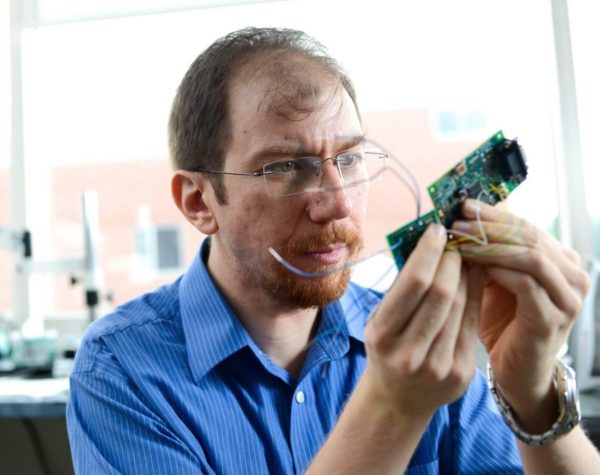
Edgar Lobaton and Alper Bozkurt, associate professors in the Department of Electrical and Computer Engineering, are working to improve wearable health-monitoring devices, on a research project that could lead to people being able to detect an asthma attack sooner. Lobaton, along with two UNC researchers, will receive $1 million from the National Science Foundation for their collaborative project, “A Data-Driven Approach to Enhancing Wearable Device Performance – An Early Asthma Exacerbation Detection Study.”
“What makes this project unique is that we’re focusing specifically on trying to identify when we have good signals from these types of wearable devices,” Lobaton says.
Using data collected from the devices, the team will employ machine learning “to automatically learn when we can rely on these signals” to make an accurate prediction about an asthma exacerbation (commonly known as an asthma attack).

Edgar Lobaton, Associate Professor, NC State. Lobaton’s research focus areas include robotics, computational intelligence, and communications and signal processing.
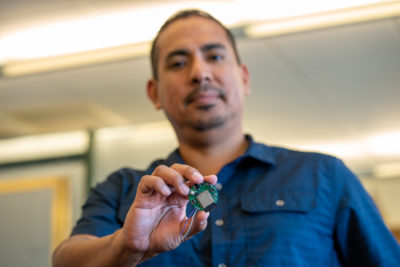
Alper Bozkurt, Associate Professor, NC State. Bozkurt’s research focus areas include bioelectronics engineering, and electronic circuits and systems.
Complementary Collaborations
This collaborative project exemplifies the complementary nature of NC State and UNC’s respective research strengths in engineering and medicine.
The collaborating researchers from UNC are Dr. Michelle Hernandez, associate professor in the School of Medicine, and Delesha Carpenter, associate professor in the Eshelman School of Pharmacy. Hernandez specializes in pediatric allergy/immunology and rheumatology, and Carpenter specializes in pharmaceutical outcomes and policy.

Dr. Michelle Hernandez, Associate Professor, UNC School of Medicine.

Delesha Carpenter, Associate Professor, UNC Eshelman School of Pharmacy
Lobaton, who won an NSF CAREER award in 2016, says the greatest value he brings to the project is his expertise and prior research in signal processing — using signals (data from a device) to create algorithms for making predictions.
Lobaton and Bozkurt met Hernandez and Carpenter through an earlier collaboration between NC State’s Center for Advanced Self-Powered Systems of Integrated Sensors and Technologies (ASSIST) and UNC, which evolved into this current project. It was during the earlier project that Bozkurt, who is also a 2016 recipient of the CAREER award, used equipment at ASSIST to develop the devices that will be used for this project.
However, the roots for this project can be traced back to 2012, when Hernandez worked with ASSIST through an NC TraCS grant that aimed to develop technology and tools for helping people manage their asthma care better and have fewer asthma attacks.
Asthma in America
According to the American College of Allergy, Asthma and Immunology, asthma attacks — inflammation and obstruction of the bronchial tubes, which make it extremely difficult to breathe — can be caused by a variety of often invisible triggers wafting through the air, from pollen to perfume. Certain illnesses and strenuous exercise can also be triggers.
The ability to quickly identify an asthma attack is crucial to effective treatment.
Over a quarter-billion Americans have asthma. And each day, asthma is responsible for roughly 10 deaths in the U.S. — most of which could be avoided with proper treatment and care.
Opportunities for Improvement in Today’s High-Tech World
Wearable technology has the potential to transform human healthcare, allowing people to constantly monitor their bodies to degrees once unimaginable. And it’s become common for young adults to use mobile, wearable devices — such as an Apple Watch or FitBit — to monitor their health. But for wearable devices to one day be able to accurately predict an event such as an asthma attack, the data they use must first be proven to be reliable. If someone is relying on a device to anticipate an asthma attack, inaccuracy could have serious consequences.
Lobaton says that, as it stands, these kinds of wearable devices generally do well under ideal conditions, like when they’re firmly secured and the wearer is sitting down. But when, for instance, someone starts running and sweat loosens this firm grip, “then all of a sudden, you start getting very erroneous measurements.”
Lobaton shows an example of the type of sensors he’ll be working with.
“The quality of the signal from the device depends not only on the device itself, but also how you’re using it, where you’re using it, and under what conditions,” Lobaton says.
That’s why Lobaton hopes this research will also lead to the ability to “give feedback to the actual device itself.” For example, if a device is not getting good signals due to reduced power consumption, the device could then recognize that and temporarily increase power consumption.
“And that’s where having access to the prototype, where we can actually change some of those parameters, will be very useful,” Lobaton says. “So we can automatically, for the next generation of sensors, learn from this data without having to rely too much on long cycles of observation.”
While this project is specifically focused on applications for asthma care, Lobaton says there are also much broader applications that could be made possible in the future.

A basic model of the kinds of health-monitoring systems that ASSIST works to develop.
For this project, the research team will collect and analyze both physiological and behavioral data. To collect this data, Lobaton says they’ll likely use a small device placed on someone’s wrist or chest as well as a slightly larger device worn on the hip. The device on the wrist or chest will monitor things such as heart rate and motion, while the one on the hip will collect data about environmental factors such as air pollution.
Taking all these different types of factors into account, the team will determine whether it’s possible to create an algorithm that accurately predicts an impending asthma attack. Hernandez and Carpenter will also use the data to assess young adults’ preferences for using wearable devices to monitor their asthma in the long term.